Others
Footwear Guide
Comfort and durability are important when selecting footwear. A shoe must conform to the shape of your foot and not vice versa. If your activities include walking long distances or standing for a long time, you must purchase shoes appropriate to those activities. Ill-fitting shoes that lack support can stress the feet, ankles, hip and spine, and lead to pain and deformities that prevent you from participating in your regular activities.
Shoes for children should accommodate the growth of the feet, and not apply pressure on the developing muscles and tendons around the ankle. Soft-soled, low-cut shoes with adequate space for the toes to wiggle are recommended. Women’s shoes should not have heels higher than 2 1/4 inches as that increases pressure on the underside of the forefoot. Regular use of pointed shoes compresses the toes and can cause deformities such as bunions and hammertoes.
There are a few important points to keep in mind when buying shoes:
- Feet usually swell towards the evening, so it is preferable to purchase shoes at this time to ensure the perfect fit.
- Measure your feet at least once a year, preferably standing up as there may be changes.
- Always try on shoes for fit and walk around in them for comfort as sizes may vary for different brands.
- There should be adequate space for your toes to wiggle and at least a half inch gap between your longest toe and the end of the shoes. Too much toe space should be avoided as it can make the feet to slip back and forth causing toe problems.
Aqua Foot Detox
The human body is exposed to various toxins through the food we eat, the water we drink and the air we breathe. Aqua Foot Detox treatment is used to detoxify and cleanse the body of these toxins.
During the foot detoxification process, you will be asked to place your feet in a tray of lukewarm water, which has a small amount of salt. The system is then switched on which produces positive and negative ions in the water. Your body absorbs these ions and neutralizes the tissue waste, which is released into the water from the feet. This is indicated by a change in the colour of the water and sedimentation. This procedure takes about 30 minutes and you will be advised to drink a lot of water after the treatment as the detoxification process continues for about 48 hours after the treatment.
Benefits of the aqua detox may include higher energy levels, healthier body, stronger immunity, less body pain, fewer allergies and improved sleep.
Lapidus Fusion
A bunion, also known as hallux valgus, is bony prominence at the base of the big toe, which often results in pain, redness and rubbing in footwear. The 1st metatarsal bone abnormally angles outward towards the other foot from its joint in the midfoot. A bunion can change the shape of your foot, make it difficult for you to find shoes that fit correctly and worsen the symptoms if left untreated.
Causes
Although it is not clearly understood why bunions occur, possible causes include:
- Family history and genetics
- Arthritis (inflammation of the joints) including rheumatoid arthritis, psoriatic arthritis and gout
- Neuromuscular conditions such as cerebral palsy (affects movement and co-ordination)
- Connective tissue disorders such as Marfan’s syndrome (affects the connective tissues)
- Tight fitting shoes that are too tight, narrow or high heeled.
- Hypermobility: Excess looseness or movement in the 1st tarso-metatarsal joint leads to instability, causing the first metatarsal bone to move in one direction. To compensate for this, the toe shifts in the other direction leading to a bunion.
Signs and symptoms
The main indication of a bunion is the pointing of the big toe towards the other toes of the foot. Other signs and symptoms include:
- Pain and swelling over the big toe that increases while wearing shoes
- Swelling with red, sore and calloused skin at the base of the big toe
- Inward turning of the big toe pushes the second toe out of place
- Bony bump at the base of the big toe
- Sore skin over the bony bump
- Difficulty walking and wearing shoes
Diagnosis
The diagnosis of a bunion includes taking a medical history and performing a physical examination to assess the extent of misalignment and damage to the soft tissues. Your surgeon will usually order weight bearing X-rays (i.e. taken while standing) to access the severity of the bunion and deformity of the toe joints.
Treatment
Mr Limaye will recommend conservative treatment measures with the goal of reducing or eliminating your foot pain.
Such measures can include:
- Medications for relieving pain and inflammation
- Wearing surgical shoes with a wide and high toe box, avoiding tight, pointed or high-heeled shoes.
- Use of orthotics to realign the bones of your foot and ease pain.
- Padding of bunions
- Ice applications several times a day
Conservative treatment measures can help relieve the discomfort of a bunion, however these measures will not prevent the bunion from becoming worse.
Surgery
Surgery is the only means of correcting a bunion. Surgery is also recommended when conservative measures fail to treat the symptoms of bunion.
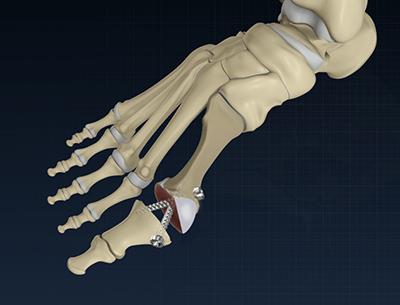
There are many surgical options to treat a bunion. A surgical procedure called the Lapidus procedure is indicated to correct a bunion caused by hypermobility of the 1st metatarsal bone. The common goal is to realign the bones in the foot, correct the deformity, and relieve pain and discomfort. The surgery is performed as a day procedure, under the effect of a light general anaesthetic and a regional nerve block. When you wake up, you will not be in pain and will be able to walk on your foot right away.
The shift in the metatarsal joint causes the imbalance in the soft tissues – elongation of medial ligaments and capsule and shortening of the lateral tissues. To correct this, an incision is made at the web between the thumb and second toe and the adductor halluces muscle, lateral joint capsule and transverse metatarsal ligament are released. Another incision is made at the first metatarsophalangeal joint. The joint capsule is opened, the bony prominence or medial eminence removed, and the capsule stitched close to the bone to tighten the slack capsule, and correct alignment of the bones.
Your surgeon either extends this incision or makes another incision along the top or middle of the toe and exposes the first tarsometatarsal joint. Underlying nerves and tendons are protected from damage. The cartilage lining the joint is removed and the bones are aligned straight. The metatarsal and medial cuneiform bone, the bones of the 1st tarsometatarsal joint, are locked or fused together. This position is held by screws and/or a plate. Bone graft may be added at the joint to further aid in healing.
Your incisions are closed with staples or sutures and the foot is covered with a padded dressing and supported by a splint or surgical shoe.
Risks and complications
As with any surgery, bunion surgery involves certain risks and complications. They include:
- Infection
- Bleeding
- Nerve and blood vessel damage
- Formation of blood clots
- Delayed healing
Post-operative care
Patients should follow all instructions given by their surgeon following the surgery. Common instructions include:
- Keep your dressings dry and leave them in place until your next outpatient appointment.
- Elevate the foot to minimise swelling as much as possible.
- Your stitches or staples will be removed in the first month.
- You will have to wear specially designed post-operative shoes to protect the wounds and assist in walking.
- You may not be able to wear regular shoes for 6 weeks
- At your next outpatient appointment, your surgeon orders X-rays to check for healing of the joint.
- Upon healing, you are allowed to slowly wean out of the post-operative shoes.
- Physical therapy is recommended to increase strength and improve range of motion in the foot.
- You can return to your normal activities in four to six months of the surgery.
It is important to note that your recovery schedule and weight bearing protocol may vary based on your surgeon’s preference.
Weil Osteotomy
Lesser toes, also called as smaller toes are those other than the big toe found in your foot. The lesser toe has three phalanx bones namely distal, middle and proximal and two phalangeal joints namely distal interphalangeal joint (DIPJ) and proximal interphalangeal joint (PIPJ). The common types of deformities that affect the lesser toes are – claw toe, hammer toe and mallet toe. Lesser toe deformities are caused due to alterations in normal anatomy which creates an imbalance between intrinsic and extrinsic muscles. The causes are wearing improper shoes, trauma, inheritance, arthritis, neuromuscular and metabolic diseases. These deformities are accompanied by severe pain and difficulty in walking and finding properly fitting shoes.
Indications
Lesser toe surgery or Weil Osteotomy is a commonly used surgical procedure to treat lesser toe deformities. Pressure under the tip of the toe, in the balls of the feet and on the corns on the top of the toes is the cause for pain in patients suffering from deformity. The callous (thick lump of skin) formation and swelling in the joints makes it difficult to walk and wear shoes. Early deformities can be treated by strapping or wearing foot wear which has silicone pads. This provides cushioning to prominent and tender areas of the foot, making you feel comfortable while you walk. If the symptoms still persist after the non-surgical treatments have been tried, surgery should be considered as the best treatment option.
Pre-surgical care
The surgeon will first diagnose the extent of the toe deformity by X-ray. After collecting the details of your medical history and the medications that you are taking, the clinical examinations will be carried out. The surgery is either performed as a day-case (no over-night stay in the hospital) or as an inpatient (with an over-night stay). The surgery is carried out under local anaesthesia combined with sedation or occasionally under general anaesthesia.
Surgical procedure
The type of surgery depends on the problem being addressed. A small incision (cut) is made across the joint and any bony bump is trimmed thoroughly. The bones may be cut and repositioned in place with the help of surgical screws, wires or staples. Your surgeon may release or lengthen the tendons. Sometimes an osteotomy (removal of bone) is necessary to fix the problem. At the end of surgery, the wound is stitched closed and covered with a loose dressing.
Post-surgical care
After the operation, you are advised to keep the foot above the level of the heart for at least 24 hours to avoid swelling. The soreness and pain will subside with the help of painkillers but might stay numb initially for 6-12 hours. The wound should be regularly dressed to avoid infection and to facilitate healing. It should be taken care that no pressure is put on the toe while walking for the first 2 weeks. You can resume your regular activities after 2 weeks, but it might take 3 months to return to normal. You will be able to drive a vehicle after 6-8 weeks and can return to sports between 3-6 months.
Risk and complications
As with any surgery, lesser toe surgery involves possible risks and complications. These can include:
- Recurrence of the deformity (occurs in 1 among 10 people)
- Swelling, stiffness and numbness
- Infection and delay in wound healing (might require antibiotics)
- Nerve damage
- Scaring
- Blood clots
In most of the patients, benefits outweigh the risks associated with surgery. This surgical procedure helps to cure the pain and discomfort while walking.
Scarf osteotomy-bunion
A Scarf osteotomy is a surgical procedure to correct a hallux valgus deformity, commonly known as a bunion. It is a very versatile procedure that allows the movement of bone across different planes.
Chevron osteotomy-bunion
A Chevron osteotomy is a type of bunion correction surgery. It is effective in treating mild-to-moderate bunion deformities.
ROTO glide total toe replacement
ROTO glide total toe replacement is a unique 3-part implant that incorporates a sliding and rotating meniscus. It has been designed to optimize anatomical movement.
Cartiva toe replacement
The Cartiva toe replacement has been approved for treatment of big toe arthritis. The implant is designed to replace damaged cartilage and reproduce natural function.
Swanson’s toe joint replacement
The Swanson Flexible Hinge Toe Implant is a double-stemmed flexible hinge implant designed to restore function to the metatarsophalangeal joints disabled by rheumatoid, degenerative, or post traumatic arthritis.
Akins osteotomy
An Akin osteotomy is a medial closing wedge osteotomy of the proximal phalanx of the great toe. It is used to correct hallux valgus deformity.
First toe MTP fusion surgery
Introduction
The metatarsophalangeal (MTP) joint connects the metatarsal bones (group of long bones in the foot) and bases of the proximal phalanges of the toes.
The MTP joint at the base of the big toe is commonly affected by osteoarthritis or rheumatoid arthritis. In cases of osteoarthritis, the surface of the joint wears out and the adjacent bone thickens and forms osteophytes (bone spurs). This eventually leads to severe pain and stiffness in the affected joint. In cases of rheumatoid arthritis the bones in the joints are extremely destroyed resulting in swelling and severe pain. These conditions may cause the MTP joint to become predominantly stiff (hallux rigidus) or deformed (hallux valgus).
Hallux arthrodesis is a surgical approach performed to fuse the MTP joint of the big toe to provide pain relief and improve function.
Indications
The affected big toe joint is initially treated with conservative approaches such as medications, physical therapy, steroid injections or exercise. Surgery is recommended if conservative approaches fail to provide pain relief. MTP joint fusion of the big toe or hallux arthrodesis is indicated in the following conditions:
- Painful joint
- Severe big toe deformity or stiffness
- Difficulty in wearing footwear
- Associated foot disorders such as inflammation, ulceration, outgrowth of bone in the joint region or nerve entrapment
Pre-operative preparation
Before the surgery, Mr Limaye may conduct a physical examination and analyse details of your medical history. Talk with Mr Limaye about any medications you are taking or plan to take. Arthrodesis is performed as a day-case procedure which doesn’t require an over-night stay in the hospital.
Procedure
The surgery is carried out under the effect of general anaesthesia or an ankle block using local anaesthetic. Your surgeon will make an incision over the big toe joint; trim the bony bump and remove the remaining degenerated cartilage around the joint surface. Your surgeon will then fuse the metatarsal bone and phalange of the big toe. The bones are held in position with the help of screws, metal staples or plates and the joint is stabilised.
Post-operative care
Following the procedure, you may have to use crutches and wear a wedge shoe for around 6 to 8 weeks in order to relieve pressure on the front area of the foot. Keep the foot clean and dry and protect it when you have a shower until the wound is completely healed. Avoid driving and long hours of standing for a few weeks. Elevate your operated foot for the first two weeks to promote healing of the wounds and to help alleviate pain. You may experience swelling of the forefoot for a few months. Exercise may be recommended to improve movement, flexibility, and to strengthen the foot.
Risks and complications
As with any surgery, hallux metatarsophalangeal joint fusion involves certain risks and complications. They include:
- Infection and swelling
- Non-healing wounds
- Nerve injury
- Malposition of the fused toe
- Rarely, deep vein thrombosis or pulmonary embolism
Correction of flat foot with internal brace
The InternalBrace can be used to correct flat foot deformity. It allows for reconstruction of the spring ligament complex which supports the medial arch of the foot.
PIP and DIP fusion toe surgery
PIP (Proximal Interphalangeal) fusion is done to correct a fixed and painful deformity of the proximal joint of the toe. DIP (Distal Interphalangeal) fusion is done to correct a fixed and painful deformity of the distal joint of the toe.
Morton’s neuroma surgery
Morton’s neuroma surgery is performed to resect a small portion of an enlarged nerve at the ball of the foot. It is usually located between the 3rd and 4th toes.
Midfoot fusion surgery
Tarsometatarsal joint refers to the region found in the middle of the foot. It is also called as Lisfranc joints. It is a junction between the tarsal bones (group of seven articulating bones in the foot) and metatarsal bones (a group of five long bones in the foot). A deformity in the tarsometatarsal region can be due to arthritis and traumatic motor accidents. Tarsometatarsal fusion is a surgery used to treat deformity in the tarsometatarsal region. During this procedure, tarsometatarsal joints (one or more small joints in the middle of the foot) will be fused together and made stiff.
Indications
Tarsometatarsal arthritis is characterised by pain, functional impairment and midfoot instability. The appearance of bruises and swelling on the dorsal side of the midfoot are the commonly observed symptoms. The early stages of injury can be treated by analgesics, steroid injections and by wearing special footwear or casts. Tarsometatarsal joint fusion is recommended if all the non-surgical procedures fail to show efficacy in treating the injury.
Pre-surgical care
The pre-operative assessment usually takes 2-6 weeks. The doctor will first examine the physical condition of the foot by inspection and palpation (feeling with hands). You may be advised to get an X-ray taken. You might also be sent to get a CT or MRI scan done to provide more information about your condition.
Surgical procedure
The surgery is conducted under general anaesthesia. One or more cuts of 3-4 cm are made on the upper or inner surface of the foot. The joints which are to be fused are opened up, reshaped and fixed together with the help of metal pins, screws or staples. The wound is the stitched closed and a plaster cast is applied from knee to toe (removed after 10-14 days). Bone grafting might be done in case of any gaps during the fusion. The bone graft can be selected from either the pelvis or tibia bone (strong bone below the knee).
Post-surgery care
In addition to general anaesthesia (during surgery), local anaesthesia may be given to reduce the pain (postoperatively) or pain killers can also be advised. You will be asked to keep the foot above the level of the heart to avoid swelling. The wound should be regularly dressed and kept clean and dry to prevent infection. You will have to wear a boot for 12 weeks post-surgery and walk with the help of crutches or a walker. It might take 6-9 months to get back to the normal daily activity, play sports and drive a vehicle.
Risk and complications
As with any surgery, risks and complications can occur and include:
- Swelling
- Infection
- Nerve damage
- Pain
- Blood clot
Ankle osteotomy
An ankle osteotomy is a surgical procedure that involves removal of a portion of the bone in the ankle. It is usually performed to correct deformities and improve function of the ankle.
Cavus foot surgery
Cavus foot is a condition in which the foot has a very high arch. Because of this high arch, an excessive amount of weight is placed on the ball and heel of the foot when walking or standing. Cavus foot can lead to a variety of signs and symptoms, such as pain and instability. It can develop at any age and can occur in one or both feet.
Causes
Cavus foot is often caused by a neurologic disorder or other medical condition such as cerebral palsy, Charcot-Marie-Tooth disease, spina bifida, polio, muscular dystrophy, or stroke. In other cases of cavus foot, the high arch may represent an inherited structural abnormality.
An accurate diagnosis is important because the underlying cause of cavus foot largely determines its future course. If the high arch is due to a neurologic disorder or other medical condition, it is likely to progressively worsen. On the other hand, cases of cavus foot that do not result from neurologic disorders usually do not change in appearance.
Symptoms
The arch of a cavus foot will appear high even when standing. In addition, one or more of the following symptoms may be present:
- Hammertoes (bent toes) or claw toes (toes clenched like a fist)
- Calluses on the ball, side, or heel of the foot
- Pain when standing or walking
- An unstable foot due to the heel tilting inward, which can lead to ankle sprains
Some people with cavus foot may also experience foot drop, a weakness of the muscles in the foot and ankle that results in dragging the foot when taking a step. Foot drop is usually a sign of an underlying neurologic condition.
Diagnosis
Diagnosis of cavus foot includes a review of the patient’s family history. The foot and ankle surgeon examine the foot, looking for a high arch and possible calluses, hammertoes, and claw toes. The foot is tested for muscle strength, and the patient’s walking pattern and coordination are observed. If a neurologic condition appears to be present, the entire limb may be examined. The surgeon may also study the pattern of wear on the patient's shoes.
X-rays are sometimes ordered to further assess the condition. In addition, the surgeon may refer the patient to a neurologist for a complete neurologic evaluation.
Non-Surgical Treatment
Non-surgical treatment of cavus foot may include one or more of the following options:
- Orthotic devices. Custom orthotic devices that fit into the shoe can be beneficial because they provide stability and cushioning to the foot.
- Shoe modifications. High-topped shoes support the ankle, and shoes with heels a little wider on the bottom add stability.
- Bracing. The surgeon may recommend a brace to help keep the foot and ankle stable. Bracing is also useful in managing foot drop.
When is Surgery Needed?
If non-surgical treatment fails to adequately relieve pain and improve stability, surgery may be needed to decrease pain, increase stability, and compensate for weakness in the foot.
The surgeon will choose the best surgical procedure or combination of procedures based on the patient’s individual case. In some cases where an underlying neurologic problem exists, surgery may be needed again in the future due to the progression of the disorder.
Surgeries for cavus foot
Surgery for cavus foot is complex, and often requires two operations performed two weeks apart or even in the same stage.
In the first operation, releases the tightest of the soft tissues in the arch is done. The rest of the tissues relax during the following two weeks.
In the second operation, the doctor cuts and reshapes at least one bone using a bony surgery and moves several tendons to new locations on the foot to improve muscle balance.
Sometimes in addition to tendon transfers, bony cuts and reshaping is required. Post operatively this is treated in a plaster cast.
Flatfoot surgery- FDL tendon transfer
The FDL tendon transfer is indicated in patients that have an acquired and flexible flat foot deformity. The goal of the procedure is to relieve pain and restore the arch.
Tendoscopy of TA
Tendoscopy is a procedure that allows Mr Limaye your doctor to see inside the tendon sheath. It can be used to identify and treat problems of the tibialis anterior tendon.
TendoAchillis repair and FHL transfer surgery
A flexor hallucis longus tendon transfer may be used to treat Achilles tendinopathy. The FHL tendon is excised and transferred into a tunnel of the calcaneous bone.
Calcaneal fracture fixation
Calcaneal fracture fixation is performed to reconstruct normal anatomy and mobility of the heel. Special screws are placed through small incisions achieve fixation of the fracture.
Excision of bony lumps/soft tissue swellings around foot and ankle
Bony lumps/soft tissue swellings around the food and ankle are usually benign. Excision is performed in case of severe discomfort or malignancy and can usually be performed in the outpatient setting under local anaesthesia.
Assessment of paediatric foot deformity
Paediatric foot deformities in children include cavus foot, tarsal coalition, & clubfoot. Evaluation and treatment of such conditions takes into account the need to maintain the integrity of the growth plates to allow normal growth of the foot and ankle.
Treatment of tendon disorders by tendon transfer
A tendon transfer is usually performed to restore normal mobility and function in a joint. Foot and ankle tendon transfers make it easier for patient to stand, wear shoes, and walk.
Click on the topics below to find out more from the orthopaedic connection website of American Academy of Orthopaedic Surgeons.
- Achilles tendon
- Adult (Acquired) Flatfoot
- Arthritis of the Foot and Ankle
- Ankle Fractures
- Athletic Shoes
- Rotura de tobillo (Broken Ankle)
- Broken Ankle
- Bunions
- Clubfoot
- Corns
- Diabetic foot
- Flexible flatfoot in children
- Foot Pain
- Fracture of the Talus
- Fractures of the Heel
- Hammer toe
- Heel Pain
- Ingrown Toenail
- Intoeing
- Orthotic Devices
- Paediatric Thigh Bone Fracture
- Plantar fasciitis
- Posterior Tibial Tendon Dysfunction
- Rheumatoid Arthritis of the Foot and Ankle
- Sesamoiditis
- Sprained Ankle
- Stiff Big Toe (Hallux rigidus)
- Stress Fractures of the Foot and Ankle
- Toe and Forefoot Fractures
